“A balanced diet is a cookie in each hand.” Barbara Johnson
“Don’t wreck a sublime chocolate experience by feeling guilty.” Lora Brody
Introduction: Have you sometimes wondered why you really wanted dessert after dinner? Or have you been thinking lately of something sweet to snack on? Well, now, you can blame it on your Parkinson’s. Palavra et al. (2021) reported that people (person)-with-Parkinson’s (PwP) had increased sugar consumption compared to healthy controls [Palavra, Natalie C., Michal Lubomski, Victoria M. Flood, Ryan L. Davis, and Carolyn M. Sue. “Increased added sugar consumption is common in Parkinson’s disease.” Frontiers in Nutrition 8 (2021): 628845.]. If you are interested in this phenomenon, read on.

Goal of the Study: To better understand the dietary habits of PwP. This study represents the nutrition in an Australian Parkinson’s cohort.
“Don’t wreck a sublime chocolate experience by feeling guilty.” Lora Brody
The Collection of Data: Each PwP and healthy control recruited for the study completed a 145-item, semi-quantitative food frequency questionnaire. The goal was to evaluate dietary and lifestyle tendencies. There was a nine-category frequency scale for the frequency of consumption of food items, which also included portion size. They performed nutrient analysis for energy, protein, carbohydrates, sugars, fats, and fiber. They had an “added sugar” category, including sucrose, fructose, dextrose, lactose, and sugar syrup. A category was also used for “free sugars,” which includes things like honey and fruit juice. They also collected demographic data and assessed quality of life using the PDQ-39 questionnaire. Furthermore, they measured motor symptoms using the MDS-UPDRS III and the Modified Hoehn &Yahr scale. At the same time, non-motor symtpoms were calculated using the Non-Motor Symptoms Scale (NMSS).
“Seize the moment. Remember all those women on the ‘Titanic’ who waved off the dessert cart.” Erma Bombeck
The Characteristics of the PwP Compared to the Healthy Control (HC) Group: 103 PwP were studied compared to 81 HC. BMI for both groups was similar, with ~5% reporting diabetes with no difference between the two groups. The PwP had more chronic pain, more depression, and more constipation, and the PwP undertook considerably less physical activity compared to the HC group. Please note that the quality of this paper is in their statistical analysis and description of their study. I am giving you the trends, not the absolute numbers reported. Again, please refer to the manuscript if you are interested in getting the full details and significant values reported.
“Strength is the capacity to break a chocolate bar into four pieces with your bare hands – and then eat just one of the pieces.” Judith Viorst
Dietary Characteristics: Mean Daily energy intake was similar for both groups. However, PwP reported greater carbohydrate intake than the HC group, which was shown to be primarily an increase in sugar consumption. The main contributors to free sugars consist of chocolate, jam/marmalade/honey, cordial, sugar, soft drinks, cake, cold breakfast cereal, and yogurt.
Figure 1 (shown below) describes that PwP consumed less protein than the HC group, although they consumed more carbohydrates and added sugar. In addition, PwP consumed more total sugars and more free sugars.
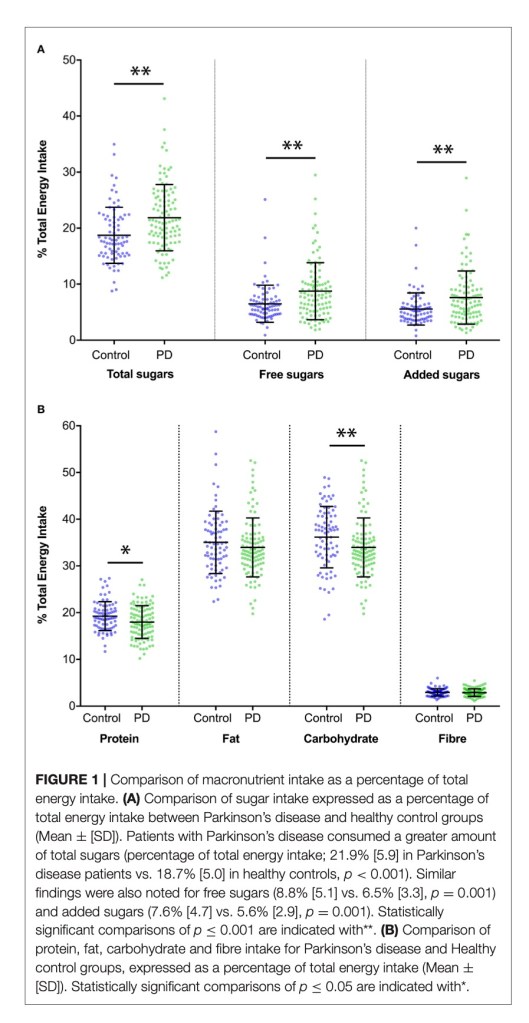
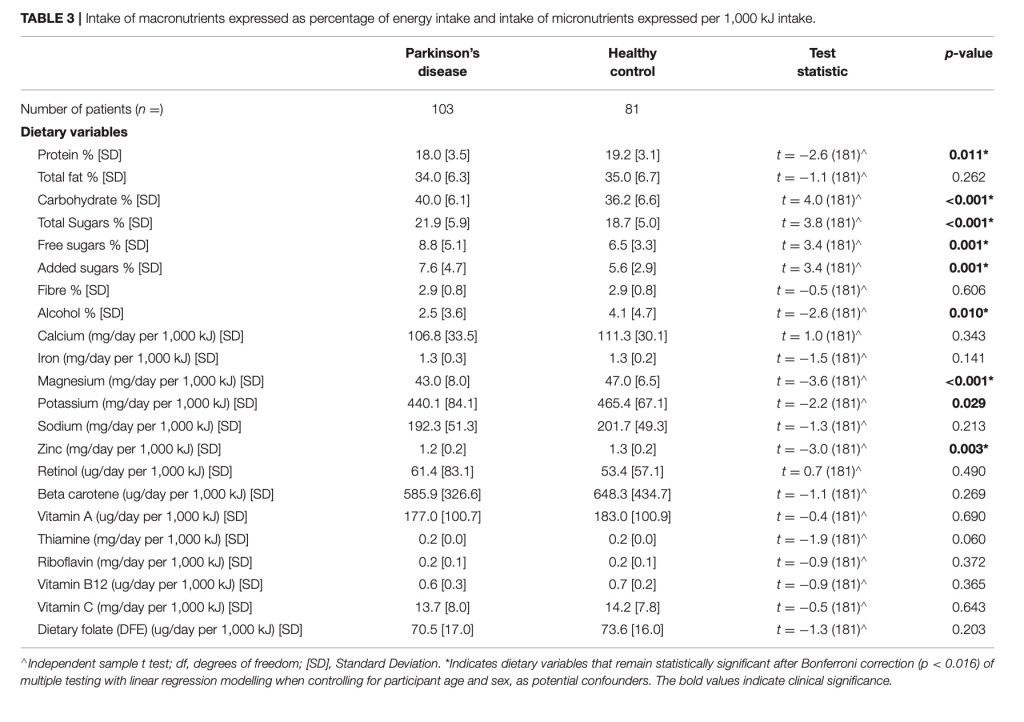
Table 3 shows a detailed analysis and macronutrient intake calculated as a percentage of total energy intake. As shown in Figure 1, they found that PwP consumed less protein than the HC group. When assessing micronutrients, they found that PwP consumed less magnesium, potassium, and zinc than the HC group.
“After eating chocolate you feel godlike, as though you can conquer enemies, lead armies, entice lovers.” Emily Luchetti
Highlighting Some Clinical Features that Increased Sugar Consumption:
•Impulse control disorder (ICD) patients showed greater energy intake than PwP without ICD. The difference was mainly attributable to carbohydrates., especially total sugar intake. Interestingly, PwP with ICD, when compared to PwP without ICD, consumed more potassium, beta-carotene, and vitamin C.
•Depression: PwP who were depressed consumed more added sugars compared to those who were not depressed. Interestingly, PwP with depression drank less alcohol than PwP without depression.
•Cognition: PwP who met the criterion for Parkinson’s dementia consumed significantly more total sugar per day than PwP without a cognition defect.
•Chronic Pain and Other Clinical Features: PwP experiencing chronic pain consumed more total sugar than PwP without chronic pain. Additionally, PwP with REM sleep disorder (RBD) consumed significantly more total sugar than PwP without RBD.
•Additional Clinical Features: PwP with higher PDQ-39 scores were associated with lower total alcohol consumption and higher total sugar consumption. Additionally, increased constipation severity was associated with increased free and added sugar consumption. Furthermore, increased total sugar consumption was associated with a more significant daily levodopa requirement. In addition, the PwP with higher NMSS total scores were found to have higher total fat intake, increased protein consumption, and overall higher mean energy intake.
“Without ice cream there would be darkness and chaos.” Don Kardong
The Deviant Nature of Parkinson’s: Every day, we learn something new that adds to the list of evils associated with Parkinson’s. I found this work remarkably helpful in exploring a new facet of Parkinson’s: the role of increased sugar consumption. The depth of the detail presented by Palavra et al. (2021) was stunning, in that almost all aspects of the symptoms that evolve from Parkinson’s lead to increased sugar consumption, and in many cases, refined sugar products, the dreaded “added sugar” components. Although this study highlighted the Australian population of Parkinson’s, I assume it would be similar to the diet in the USA and much of the world today.
This study has prompted me to evaluate what I eat and why. Is Parkinson’s leading me to want to eat ice cream in the evening? If so, then I have another battleground to mount to confront my Parkinson’s. I appreciate the work shown in this paper. It gives me some new ammunition to use mentally and emotionally because nothing about Parkinson’s is easy. Now, we need to add the ability of Parkinson’s to drive us to eat more sugar. Battle on, my friends. Now, be aware of your diet and its contribution to the everpresent dark side of Parkinson’s.
“The fastest growing segment of the population in the world right now is over the age of 90, and in some cases over the age of 100 in some countries. So people are living longer. And even though much of it is attributed to modern medicine, it’s not. It’s lifestyle. It’s nutrition. It’s the quality of exercise, the ability to manage stress.” Deepak Chopra



I’ve known about my “sweet tooth” for years… What I didn’t know is that perhaps,I come by it naturally!
LikeLiked by 1 person
I agree with you.
LikeLiked by 1 person
I Read this as soon as I received it. I was using sugar to help my low energy levels. I really like to read whatever information comes in on Parkinson’s,Especially when Frank Church sends it!i
Sent from Yahoo Mail for iPhone
LikeLike
Robin, thanks for your comments, Frank
LikeLike
As always Frank you are on point. I just did my bi-annual complete blood work-up. A1C came back in a diabetic state. Ketones and glucose also not good. And yes I have been a sugar-holic my whole life. No more little debbies….. 😦
LikeLike
Tommy, there is a real relationship with Parkinson’s and diabetes, we should all get our blood checked regarding glucose and A1C levels, it could make a difference, Take care, Frank
LikeLike