“The Eyes are the window to your soul.” William Shakespeare
“The eye of a human being is a microscope, which makes the world seem bigger than it really is.” Khalid Gibran
Introduction: Parkinson’s creates havoc in many areas of our bodies. This month, I had two rounds of surgery to remove cataracts (cloudy lenses). There is evidence that Parkinson’s may accelerate cataract formation above the baseline rate caused by aging.
“Our life is what our thoughts make it.” Marcus Aurelius
Dopamine and Eyes: Dopamine is involved in more than just motor issues. The schematic below highlight the dopamine pathways, including the eye and retina. I have previously written a blog post about the role of dopamine in vision [Parkinson’s: The Eyes Have It (click here)].
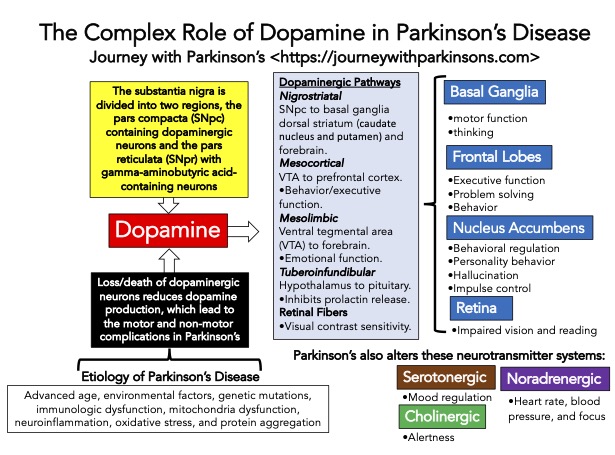
Within the eye, dopamine has several functions, including:
•light adaption;
•spatial contrast sensitivity;
•color discrimination;
•visuospatial problem solving;
•spatial working memory;
•oculomotor control;
•promotion of the photoreceptor renewal process;
•reduction of its waste product accumulation;
•may also be involved in he cyclic regulation of intraocular pressure.
“What we see depends mainly on what we look for.” John Lubbock
Parkinson’s is Known to Cause Issues with Eyes and Eyesight: The loss or reduction of dopamine in Parkinson’s in the eye has been shown to cause decreased visual acuity, contrast sensitivity, and color discrimination. Besides these features, dopamine depletion leads to poor visual function in the retinas, abnormal eye movements, and poor blinking. Importantly, there is a higher frequency of cataract formation in Parkinson’s. In post-mortem studies, increased deposits of alpha-synuclein were found on the lens of Parkinson’s patients compared to aged match normal controls.
“Sight is a faculty; seeing is an art.” George Perkins Marsh
Cataract Surgery: If your Ophthalmologist has recently told you that you have cataracts, what symptoms does one have: glare or halos at night that lead to difficulties when driving at night; blurred vision; difficulty distinguishing colors; trouble reading fine print; and potentially other changes in the quality of your eyesight. Based on your Ophthalmologist reports and your sight situation, you may decide that the diseased and cloudly lens should be replaced.
The schematic below gives a general idea behind the surgery. Removing the diseased lens and inserting the new clear lens takes about 10-15 minutes. You will likely spend more time driving to the Day-Op Surgery Center, getting ready with pre-operative issues, mainly drops in your eye to numb it, and getting an IV set up in your hand to give you a mild sedation, usually something like Versed and fentanyl. Eye drops are essential to numb your eye so you do not feel anything during the procedure, and the sedation is to calm your nerves and reduce the anxiety of eye surgery.

“A horizon is nothing save the limit of our sight.” Rossiter W. Raymond
My Experience with Cataracts and Cataract Surgery: I was told about 4-5 years ago that cataracts were forming in my eye lenses. I moved to SC 3 years ago, and I began to notice how difficult it was to drive a car in the evening—not having had my eyes checked in the last 4 years, my Family practice physician recommended a highly-regarded local Ophthalmologist. After a comprehensive 60 minute inspection of my sight, she recommended cataract surgery, as both lenses were cloudy. So, I scheduled the surgery. The surgery is scheduled two weeks apart; do one eye, recover, and then do the second eye.
Preparation for Surgery- Nothing out of the ordinary, stop eating food and drinking liquids at midnight before the surgery. They definitely said to follow my usual routine with carbidopa/levodopa and NeuPro dopamine agonist patch. The key phrase was, “Frank, you cannot move your head for 10-15 minutes.”
Pre-Op- We checked into the Day-op Surgery Center at 6:30 AM; after filling out some forms, I was brought back to the room to prepare for surgery. Fully dressed and only told to wear a button-down shirt to allow for placement for a few electrodes, etc., they gave me a warm blanket, took my blood pressure and temperature, and put a small stent on the top of my hand. They then began eye drops on my right eye, several times. At some point, they used mild sedation (I think it was a small amount of Versed and ketamine) and they wheeled me into the operating room.
Surgery– They positioned me on the bed, made me as comfortable as possible, and then began. After placing the new lens in my eye, they asked me to focus on pairs of red lights, which ensured the correct placement in the lens. They covered my eye with a protective plastic shield, taped me up, and the procedure was done in ~10-15 minutes. I was then wheeled to the recovery room.
Recovery room- They gave me two Tylenol and, an antibiotic pill, and some Diet Coke to down the pills. Then I walked out to Susan in the car, waiting outside to head home. My stay in recovery was about 10-15 minutes.
Recovery– I was a little dizzy during the day (a potential side effect of one of the sedatives), had a bandage over the eye, and just stayed home and relaxed. The following day at 7:30 AM, I had a follow-up appointment with the surgeon. They removed the bandage covering my eye, and my first view was good but a little cloudy. After about 5 minutes, my vision had cleared and was down to about 20/25 (20/20 vision is what we call normal vision). I was told to keep using the eyedrops three times per day with 1 drop in the eye. And now the wait for two weeks until the left eye was done. I was also told to do no heavy lifting, no golf, and nothing strenuous while the eye healed. But I got used to it. Two weeks in limbo because I could see out of one eye with the new lens just fine and my left eye was still the same as before.
I have worn eye glasses or contact lenses since I was 18. I remember distinctly being 40 years old and coming out of a subway in Paris, France, and not being able to read the city map without pushing my arms out a little further. I switched to bifocal glasses. Thus, this first operation repaired my vision to near normal, which I could not manage without wearing corrective lenses.
Two weeks later- I repeated the entire process again, with the same great results.
“Sight is about what lies right in front of us. Vision is what lies ahead.” Thomas Haden Church
Parkinson’s and Cataract Surgery: A big concern of mine from the beginning was the potential risk of cataract surgery for someone with Parkinson’s. I was lucky that my Ophthalmologist had fully assessed the situation during my initial vision evaluation. She said that I do not have a head tremor and that as long as I was optimally medicated with carbidopa/levodopa and the NeuPro patch, she was not concerned. She also said the sedatives were very mild and should not alter my respiratory system during the procedure.
I did not approach my Neurologist with this issue of cataract surgery and having Parkinson’s. As usual, this post is NOT meant to give medical advice; I am just reporting my experience. If you have cataracts and Parkinson’s, please consult with your Ophthalmologist and Neurologist; their opinions about your physical status will go far in helping you decide about this surgical procedure. The gift of sight is precious, and I am thankful I had the procedure done.
“Our sight is the most perfect and most delightful of all our senses. It fills the mind with the largest variety of ideas, converses with its objects at the greatest distance, and continues the longest in action without being tired or satiated with its proper enjoyments.” Joseph Addison
References:
Lai, Shih-Wei, Cheng-Li Lin, Kuan-Fu Liao, and Kao-Chi Chang-Ou. “Increased risk of Parkinson’s disease in cataract patients: a population-based cohort study.” Parkinsonism & related disorders 21, no. 1 (2015): 68-71.
Chiew, Alyssa, David Mathew, Chandra M. Kumar, Edwin Seet, Farnad Imani, and Seyed-Hossein Khademi. “Anesthetic considerations for cataract surgery in patients with Parkinson’s disease: A narrative review.” Anesthesiology and Pain Medicine 13, no. 3 (2023): e136093.
Thacker, Minal, Ka Ying Wong, Liping Zhou, Juewen Liu, and Man-Sau Wong. “Exploring Ocular Disorders in Parkinson’s Disease: A Comprehensive Review and Future Perspectives.” Experimental Eye Research (2024): 110225.
Hamedani, Ali G., Danielle S. Abraham, Maureen G. Maguire, and Allison W. Willis. “Visual impairment is more common in Parkinson’s disease and is a risk factor for poor health outcomes.” Movement Disorders 35, no. 9 (2020): 1542-1549.
Hamedani, Ali G., Danielle S. Abraham, Maureen G. Maguire, and Allison W. Willis. “Visual impairment is more common in Parkinson’s disease and is a risk factor for poor health outcomes.” Movement Disorders 35, no. 9 (2020): 1542-1549.
Ekker, Merel S., Sabine Janssen, Klaus Seppi, Werner Poewe, Nienke M. de Vries, Thomas Theelen, Jorik Nonnekes, and Bastiaan R. Bloem. “Ocular and visual disorders in Parkinson’s disease: common but frequently overlooked.” Parkinsonism & related disorders 40 (2017): 1-10.
Nowacka, Barbara, Wojciech Lubiński, Krystyna Honczarenko, Andrzej Potemkowski, and Krzysztof Safranow. “Ophthalmological features of Parkinson disease.” Medical science monitor: international medical journal of experimental and clinical research 20 (2014): 2243.


