“I don’t like surgery. I don’t like elective surgery, I don’t like surgery that you have to have.” Sandra Bernhard
“Truth, like surgery, may hurt, but it cures.” Han Suyin
Précis: On Wednesday, May 28, 2025, I had total hip replacement surgery on my right hip. Why talk about hip surgery when the blog focuses on Parkinson’s? Because a lot of people-with-Parkinson’s also will develop arthritis in some of their major joints (hips, knees, shoulders) and may eventually require surgery to replace the painful joint. Why do we need another testimonial/description of hip replacement surgery? Over the last few weeks, I have read and watched numerous videos, blog reports and updates about someone’s hip replacement surgery. Each one was similar to the others, but each also had a few tidbits of information not included in the other presentations. Thus, considered together, they were all collectively educational and valuable.
“I haven’t had any problems with my back since I got the foot surgery.” Merle Haggard
Risk Assessment of Surgery and the Patient: A few weeks before my surgery, my orthopedic surgeon requested a form completed by my primary care physician, which reported my overall health and ability to undergo major surgery, such as hip replacement. During the meeting with my Primary Care Physician, we filled out a two-page form together. Ultimately, this assessment determined the type of surgery I was undergoing and whether I was a suitable candidate for it. Little did I know that there is a “Risk Stratification Index” considering the patient and the type of elective surgery. The assessment is based on a scale of 1-5, ranging from Very Low Risk to Very High Risk. Major joint replacement surgery (hip, knee, and shoulder) is considered to be in category four or High Risk. Interestingly, after a review of my overall health, I was considered to be in category four as well, a High Risk patient, not because of my Parkinson’s but because I have Obstructive Sleep Apnea.
“Don’t cut bangs with a hatchet. Don’t do brain surgery with a pickax.” Joanne Greenberg
Preparing for Hip Replacement Surgery: Three years ago this month. I retired, and we moved to the “Lowcountry” region of South Carolina. During that summer, I visited my first Orthopedic surgeon to look at my right knee. Along with the knee pain, I was also having hip and lower back pain/issues. From the X-rays, he explained that I likely needed knee surgery and would possibly need hip surgery from looking at the amount of arthritis in the right hip joint.
I had right knee surgery in the summer of 2024, bilateral removal of meniscus cartilage; however, my hip pain had progressed along with the lower back pain. I dealt with the back pain with another Orthopedic physician who specialized in spinal disorders. We dealt with the back by occasionally injecting anti-inflammatory agents into the L4-L5 region of the spine. The knee was initially fine following surgery; however, over the past year, it had begun experiencing new pain. My newest physical therapist (PT) and I reasoned that the hip dysfunction was influencing both the knee and lower back pain. Hopefully, the surgery would give me a new functional hip joint and lessen the pain in my knee and back.
Early this year, I visited four different Orthopedic surgeons about my hip, and they all agreed it needed to be replaced. Furthermore, they were each asked the same question: “How would you deal with a patient needing a total hip replacement who also has Parkinson’s disease?” The orthopedic surgeon I chose provided the most cogent and logical response, which I found to be of utmost importance. It made sense to me, and I said, “Let’s schedule the surgery.” Initially set for March, we had several travel plans set for March, April, and May; we re-scheduled the surgery for late May.
“I was going to have cosmetic surgery until I noticed that the doctor’s office was full of portraits by Picasso.” Rita Rudner
The Week Before Hip Replacement Surgery: We met with the Orthopedic surgeon’s Physician Assistant, and he was going to assist during the surgery. He was intelligent and well-focused and told us everything we needed to know about the surgery. He was most likable and made me feel good, not nervous, about the surgery.
I needed to stop all of my supplements, but importantly, keep taking my Parkinson’s-specific medications. Blood work was needed to assess complete blood count (CBC), kidney and liver function, coagulation screens, and an electrocardiogram (EKG). The following day, we had appointments at the hospital to review the protocols for the surgery. We should plan on being there for 5-6 hours and show that I could walk and function independently to the hospital’s physical therapist. I would then be able to leave and go home. Otherwise, I would be required to spend the night in the hospital. Thus, I was determined to walk after the surgery.
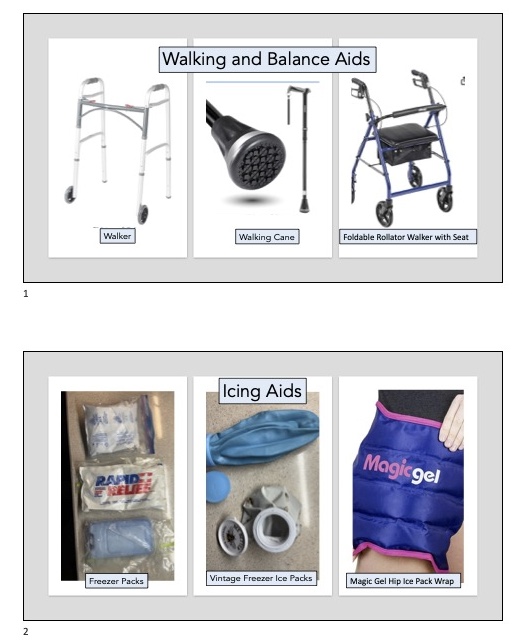
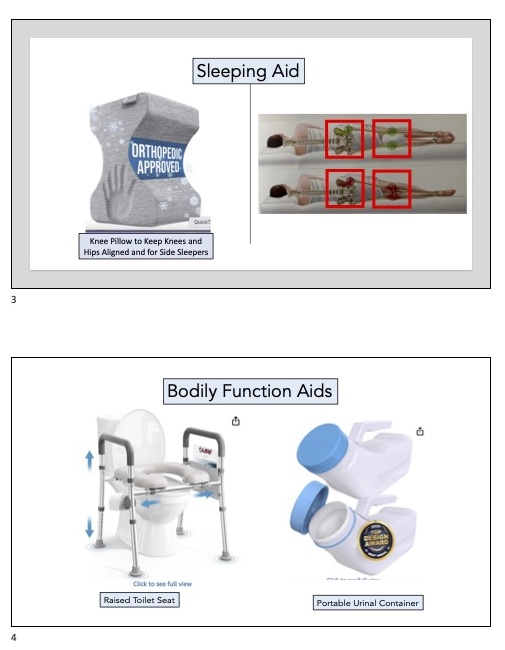
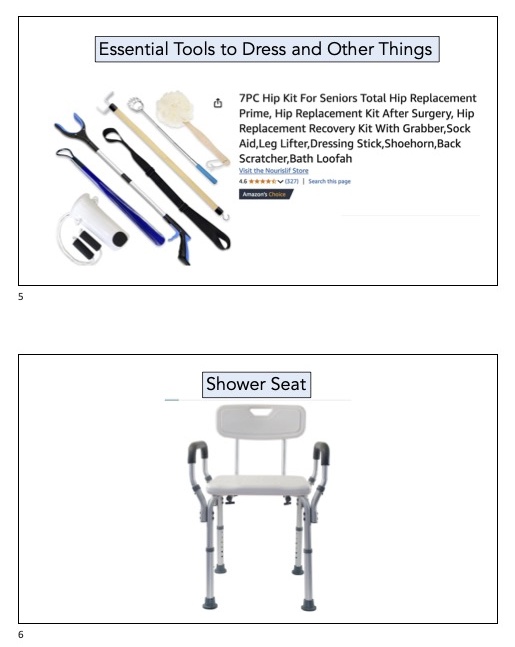
The home health group sent me a walker and elevated bedside commode (I set it up in the bathroom). Pictured below are the other pieces of equipment I purchased to aid in my recovery. Everything shown has been used on a daily basis: walking and balance aids, icing aids, sleeping aid, daily function aids, tools to help you get dressed, anti-embolism stockings, and an assortment of prescription (including two narcotic drugs) and OTC items to help manage the inflammation, swelling, and pain during recovery and rehabilitation time.

The day before surgery, all the above things should be in place and ready to use. I was to shower in the morning and evening with Hibiclens (antibacterial soap), ensure that there were clean linens on the bed, and designate an area as mine in the house with everything I would need for the day close at hand. Avoid heavy labor the day before to ensure there are no cuts or scratches on the legs, as surgery would be canceled if any occurred on the right leg. Stop eating food by midnight, and drink a bottle of Gatorade or Powerade between midnight and 2 hours before my scheduled arrival time at the hospital.
“I got the bill for my surgery. Now I know what those doctors were wearing masks for.” James H. Bor
The Day of Hip Replacement Surgery: Everyone at Hilton Head Hospital was nice and ready for or arrival at 7:45 AM. With an expected start of the surgery at ~9:45 AM, I first checked into the pre-op area. This was when I changed into a hospital gown, had an IV started, my blood pressure monitored, and a large family history was completed with two nurses working with me and also asking questions. We met briefly with the Surgeon, and then I was transferred to the Anastheia pre-op area, where I met and was questioned by a Nurse, the Anesthesiologist, and the Nurse Anesthetist. From there, I went to the OR. The next thing I remember is waking up in Recovery. Susan was there, telling me that all had gone well (the Surgeon had spoken with her in the waiting room). Eventually, they brought me to the original pre-op area, where I spent time with another Nurse and a hospital PT, who was there to assess my ability to walk.
I had to prove to the hospital physical therapist that I could walk before being discharged from the hospital. The muscles in my leg were listless, so with Susan’s help, we guided my leg along the top of the bed. Susan has been by my side throughout this journey, and she has been instrumental in my recovery. Once at the edge of the bed, I used my arms to push up to stand. Yay! Then, with the walker, I made it to the men’s room to use the restroom. Then, with the walker, I walked back to the bed. Small gains lead to a faster recovery. From there, I received instructions on how to get into/get out of a bed, enter/exit a car, and use some of the tools needed to dress each day (so I had duplicates of some of the devices/tools to facilitate dressing). I was made to understand that the seven drugs I had at home were to be taken for the expected time periods, and to use pain as a key marker of when to go to use the narcotic drugs and in what order of use. The biggest fear following surgery includes some obvious features, such as infection and thrombosis. The biggest hurdle to overcome is the fear of joint dislocation, which is addressed in the next section.
Medications to be Used for Pain, Inflammation and to Reduce the Risk of Thrombosis
| Medication | Dose and Frequency | Function |
| Baby Aspirin (81 mg) | 1 tablet, twice per day for 6 weeks | Anti-inflammatory and anti-coagulant (inactivates blood platelets) |
| Tylenol (500 mg tablets) | 2 tablets,3 times per day for 6 weeks | Anti-inflammatory and use for mild pain |
| Celebrex (200 mg capsule) | 1 capsule at night for 2 weeks | Treat mild pain and inflammation |
| Prednisone (2.5 mg pill) | 1 pill in the morning for 2 weeks | Reduce inflammation and suppress an overactive immune system |
| Tranexamic acid (650 mg tablet) | 1 tablet twice per day for 2 weeks | Prevents bleeding, it is an antifibrinolytic, meaning it prevents the breakdown of blood clots. |
| Tramadol (50 mg tablet) | Take 1-2 tablets every 6 hours (remember this is a narcotic drug) to manage moderate pain | If pain cannot be managed by the above drugs, take Tramadol (maximum of 4 doses in a 24 h period |
| Oxycodone (5 mg tablet) | Take this narcotic drug as needed every 4 hrs to manage severe pain | For extreme pain, take 1 5-mg tablet first, then take 2 tablets as pain ramps up (maximum of 6 doses in a 24-hour period) |
“Like the old Italian saying goes, ‘It ain’t rocket surgery.” Nadia Giosia
Managing the Ten Days After Hip Replacement Surgery: You leave the hospital with a simple set of rules; however, they need to be followed explicitly for the first six weeks. Managing to avoid these hip precautions takes some due diligence, much practice, and frequent reminders. As stated, you cannot bend over, never go past 90 degrees back-to-leg, never twist, and use ice and elevation constantly to reduce swelling and, subsequently, pain. The details are given below in the Table.
| Hip Precautions | What NOT to do or Avoid Doing |
| Avoid flexing the hip joint past 90 degrees (the most important guideline) | • Do not rock out of a chair, use your arms to press straight up; •Only put your shoes/socks on with the grabber, do NOT bend over; •Do not pic up things off the floor without using the grabber tool; •Avoid sitting on very low seats like a couch. |
| Avoid adducting the leg past the middle of your body | •Do not cross your legs; •Do not twist your torso over your legs •Try to keep your chest in a straight line with your legs. |
| Avoid internal rotation of the hip past neutral. | •When raising your leg, keep your leg straight and point your toes straight ahead or to the outside; never point your toes inward; •When putting on socks and shoes in a seated position, avoid reaching down and to the side, as this internally rotates and adducts the hip in an unsafe manner. •When seated or standing, avoid twisting your torso while keeping your feet and legs planted on the ground, and maintain a straight line with your whole body. |
| Your hip and leg will swell. As a result of the swelling, your hip and leg will hurt. | To •avoid the swelling and subsequent pain, ice your hip and leg for 20-30 min every hour. •To further help ease swelling and pain, keep your leg elevated at all times. • The only time the leg should not be elevated is when walking, during therapy, using the bathroom, and when eating. |
Your goal for the first six weeks is to manage the new hip by following these guidelines. This includes avoiding specific movements, learning how to dress and undress with the use of tools, taking medication to control pain, and reducing swelling with ice and elevation. By adhering to these guidelines, you, as an active participant in your recovery, will be now living in less than the constant pain and dysfunction you had before surgery.
Days 1 and 2: We arrived home early in the afternoon, and I indulged in a 3-4 hr nap. My pain level was a mere 4-5 (on a scale from 1-10), a significant relief from the 8-9 I’ve been enduring for the past several months. The best part? It’s only my new hip joint that’s causing discomfort, not my groin, thigh, buttocks, or lower back muscles.
Day two started remarkably well; I experienced some pain, swelling, and stiffness, but it wasn’t too bad. However, they had injected me with several anti-inflammatory agents in the hip area as they were closing the leg. Therefore, the next few days were likely to be different as these drugs lost their effectiveness.
The first Home Care person visited on Day 2 and just wanted to ensure we had everything set up. She took my blood pressure (which was relatively low for me) and my heart rate and then asked me to show her how to get in and out of bed. She inspected the bandage on my hip and, after seeing neither blood nor any oozing, gave me the go-ahead to begin showering and bathing again.
Days 3 and 4: My surgeon had predicted these two “hard hurt” days, and he was not kidding! The hip and leg were quite swollen. The pain was intolerable, and I felt like someone had placed a vice on my leg and just kept pressing down harder and harder. I had to move up to the narcotics [Tramadol and Oxycodon (taking only 1/2 tablet of Oxycodon)] to manage the pain. Ice and elevation were used, but they did not alleviate the severe pain. The pain started that night, and lasted for for 2 days, it was the worst pain I had ever felt. Both the surgeon and his PA said, “Don’t fear the pain; use the narcotic drugs to manage it, and see how they work.” And they worked well. Day 4 did not change much; narcotics were necessary to stay alive, it seemed.
The home Physical therapist visited on Day 3. He took my pulse rate and blood pressure (again, lower than usual for me). He gave me six simple exercises to do daily, including getting up and walking for 5 minutes every hour. That is all the therapy my surgeon believes in for the first few weeks. I also realized that the bed had an adjustment that would allow the foot region to be elevated, thus making sleep more straightforward and helping facilitate drainage of excess fluid in my leg back to the heart (this started making a difference).
Day 5: Waking up to the maximal degree of swollen leg, the pain was slightly down, and for most of the day, I did not need either of the narcotic drugs. I wandered into my office to get my email. I started reading about the experiences of others in managing their post-operative pain. I was getting ready to do my exercises, and as I began to stand up from my chair, it moved away from me. I could not reach my cane, and I fell to the floor on my left hip. I sat there for a few minutes, making sure everything was ok and trying to assess what the crap had just happened. I realized that the socks that I had on were slippery, the rollers on my chair did not lock, I was unaware of my immediate location to find either my roller or cane to help me get out of my chair, and my mind went lax for a few seconds (I was tired and in need of a nap), and I fell. I was demoralized for the rest of the day; this was my first fall since my diagnosis of Parkinson’s, going on 14 years. Now when asked by my Neurologist, had I fallen recently, my answer would be yes. I did end up taking a Tramadol that evening to manage the pain and to help me sleep.
Day 6: The swelling was coming down, along with the pain. Random bruises appeared on my leg (as predicted by my healthcare team) and some leg pain and stiffness. But nothing like the first 5 days. My mind was clear, but I also felt exhausted by the end of the day. My routine consisted of at least 30 minutes of ice on the hip and knee per hour, done four to five times per day, a nap for 1-2 hours in the afternoon, and walking as much as I could inside my house (using the cane instead of the rotating walker). And I would try to do my exercises once, maybe twice per day, ensuring I was committed to my recovery.
I felt good enough to go and get some lunch away from home. Susan and I had a lunch date. I ws exhausted by the end of lunch and came home to take a nap.
Days 7-10: The swelling had continue to recede, and the pain has dropped dramatically. The leg feels better, almost back to normal, and its form and function are returning. However, I am far from normal, but I have been forgetting to use my cane or walker today.
Susan thinks I must be an anomaly or something to have progressed so far, so fast, in just over a week. The PT visited on Day 7, and he agreed that my recovery was unusual in the first week, but he was happy for me.
I am eagerly anticipating the prospect of walking outside this coming week. It’s been a period of fairly strict adherence to my recovery guidelines, and I’m committed to continuing to follow my rule book of dos and don’ts. I have complete faith in my surgeon’s expertise, and I believe that following his advice will keep me on the right path for a while longer.
Today, as I write this blog post and watch the men’s final singles match of the French Open tennis tournament, I see little swelling, and the random pain of the past few days is gone. I am hopeful for a good post-op appointment on Tuesday when we visit my Orthopedic surgeon. The golf course and hitting golf balls are still weeks away. But I am more hopeful of this future event occurring than I was a week ago when I was massively swollen in my leg and using narcotic drugs to manage the pain.
“Winning is overrated. The only time it is really important is in surgery and war.” Al McGuire
Comments About My Orthopedic Surgeon: Before meeting my surgeon, Dr. Jason P. Norcross, who is at Hilton Head Orthopedics (it recently became Novant Health Orthopedics and Sports Medicine), I read many online opinions and comments about him. Dr. Norcross was said to be caring, taking the time to listen to his patients and clearly explaining the surgical procedure. In addition to his compassionate nature, he has a reputation as an outstanding surgeon. And in-person, he was exactly as depicted on-line. One could tell how much he cared for patients, and providing us with outstanding results from surgery was an expected goal.
Upon further reading his credentials, I saw that Dr. Norcross attended the University of North Carolina at Chapel Hill (UNC-CH) for medical school. This meant that I had the pleasure of teaching him in an introductory Pathology course and the Hematology course we taught in the late 1990s. Neither of us recognized the other from that long time ago. But the reason I chose him for my surgery is that he gave the best and most logical answer to my question about hip surgery to a patient with Parkinson’s, and not because he attended UNC-CH.
“Let the writer take up surgery or bricklaying if he is interested in technique.” William Faulkner
“Let Me Live Again” (this phrase from a recent blog post, click here): If you have had hip replacement surgery, I congratulate you for enduring this process. Suppose you are anticipating having total hip replacement surgery. In that case, the pain is real, and it takes time to recover (we all individually heal at different rates). I am far from completely healed and active again; only time will tell. But to remove the constant pain and dysfunction from before the surgery, it is worth the risk. Today, I am mostly pain-free in my right hip, leg, knee, and lower back, and I have not felt this way in over two years. By completing a significant amount of physical therapy, my goal is to be back on the golf course by sometime in August.
“I don’t enjoy the diminishing agility of the body! I had knee surgery and I no longer can go do three yoga classes and run. It’s not as much fun, physically. But emotionally, it’s way more fun. I am so much happier and contented and less agitated – I’m just calmer. So it’s like everything in this human existence, it’s a trade off – it’s like you trade the virility of the body for the agility of the spirit. That’s a good line. I have to remember that!” Elizabeth Lesser
Cover Photo Credit: Frank C. Church


