Précis: I can recall this happening twice during the past 12 years. What am I talking about? It was a day where everything seemed to be “off” regarding my symptoms, primarily motor-related. Has this ever happened to you? If so, I’d like to hear how you dealt with a prolonged off-period.
A Typical “Off-On” Period: What I want to describe/discuss is NOT to be confused with the more typical “off-on” period of fluctuation that occasionally accompanies the long-term use of carbidopa/levodopa. It manifested itself after a few years of taking the “gold standard” carbidopa/levodopa, where the ‘on’ feeling peaks and then moves quickly to an ‘off’ feeling, and the motor symptoms sneak out of their hiding places. With time, as the next dose of carbidopa/levodopa starts to take hold, those pesky motor dysfunctions melt away. Once again, you are ‘on.’
Managing the More-Typical “Off-On” Period: First, eventually, most people with Parkinson’s will be treated with carbidopa/levodopa. Next, since Parkinson’s is a progressive disease, we eventually experience complications or fluctuations in our response to these daily doses of carbidopa/levodopa. This is due to the continued loss of dopaminergic neurons over time. There are several different management strategies that you have all heard about before. I refer you to the following publication for an excellent review of the different strategies for managing this off-to-on condition: Koch J. Management of OFF condition in Parkinson disease. Ment Health Clin. 2023 Dec 1;13(6):289-297. doi: 10.9740/mhc.2023.12.289. PMID: 38058599; PMCID: PMC10696172.

A Not so Typical Prolonged Off Period, The “Off” Day, Remembering the First Time: We were in California, having just spent the week traveling from San Francisco to San Jose to Carmel-by-the-Sea, and then to Pebble Beach, south down the Pacific Coast Highway to near San Luis Obispo, then up in the mountains to Paso Robles. The trip was focused on wine tasting, and it was simply amazing.
On our return to the Bay Area, we had planned to visit the Monterey Aquarium (to include some science in a vacation), and the day seemingly started as usual; I had taken the first dose of carbidopa/levodopa and the NeuPro patch. However, I felt ‘off’ without energy as we entered the Aquarium. And so the day went, stopping frequently to rest and not panic and trying to avoid bumping into the growing crowd. I took my next dose of carbidopa/levodopa; it worked a little, but it seemed like I had missed multiple doses of carbidopa/levodopa. My arm tremor shook some, the tremor in my jaw started, my brain became a fog, and I am still avoiding people. By mid-afternoon, and an accelerated next dose of carbidopa/levodopa, some clarity was coming back, motor symptoms were beginning to be put back in their resting place, and the fog in my mind cleared up. Luckily, by then, it was time to get dinner, turn in the rental car at the San Jose airport, and get ready for the all-night flight back to North Carolina on the East Coast.
Jump-Forward Six Years and a Return Visit of the Off Day: What seemed to be a typical day at home started, as usual, taking my first dose of carbidopa/levodopa and the NeuPro patch at about the time in the early morning. As I approached the second dosing schedule, I had the same feeling described above; I started feeling stiff and somewhat listless. I knew I had a Physical Therapy appointment that afternoon and felt even more stressed than before. I took the next dose of carbidopa/levodopa a little sooner than usual, and I made it through the PT session. But, this awkward feeling still existed with motor symptoms peeking out.
I made it home from PT and decided, since it was late afternoon, and I was in charge of dinner that night, I decided to get my mind away from the way I felt. I decided to bake some banana bread (the recipe is below). That helped, and by early evening, after accelerating two treatment doses a litle sooner than planned, I was returning to normal.

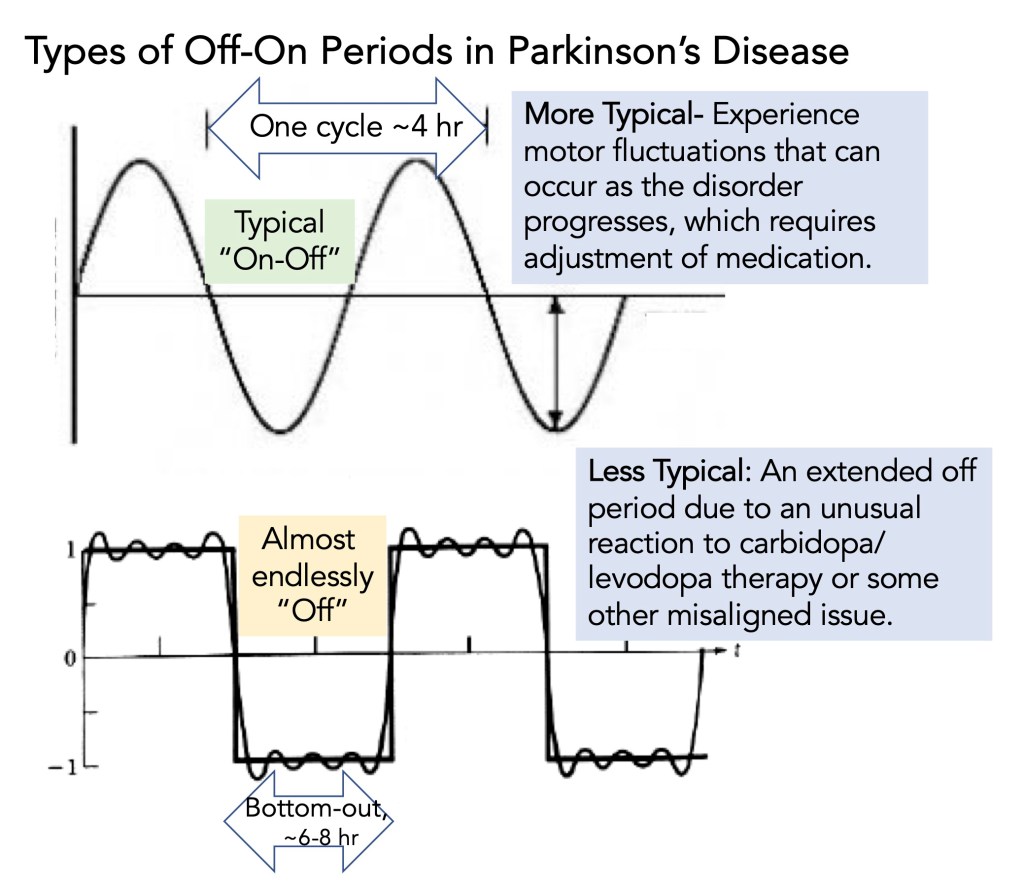
Distinguishing Between the More Typical Off-On Cycle and the Atypical Off for an Extended Period: It seems to me that one could describe the more typical cyclic off-on period using a sine wave format, where in 1 cycle, you would be on and then, potentially followed by an off phase (see drawing below). The on-cycle begins as carbidopa/levodopa gets converted to dopamine in the brain. Its concentration diminishes, which could result in some motor symptoms appearing in the off phase. By contrast, the Off day would not be cyclic; it would never rise above for an extended period and then slowly recover to normal (compare the two graphs below).
Understanding the Causes of the Off Time: The Parkinson’s Foundation offers these events as to potentially causing the ‘Off’ time (Managing “Off” Times in Parkinson’s, click here):
•Early morning “off,” before the first dose kicks in;
•Middle-of-the-night “off” when the evening dose wears off;
•Unexpected “off” not related to when you take your medication“Off” after a big or protein-rich meal;
•Delayed “on” due to constipation or slow digestion (these can affect how medication works);
•Dose failure when a single medication dose does not work at all;
•“Off” after a big or protein-rich meal.
For me, without proof, I had a dose failure that did not work at all. This put me at a deficit that led to an imbalance that my body expects for carbidopa/levodopa. This void was present, which led to the beginning of these motor symptoms turning on. Only by repeatedly taking carbidopa/levodopa doses early did this imbalance start to correct, and the motor symptoms lessened. Had I thought about it, I would have taken at least part of the dose of carbidopa/levodopa sublingually to speed up the transfer of the drug from the body to the brain. I have never been set up for emergency treatment using apomorphine, which would have been a quick way to get some improvement in the motor symptoms.
Dealing With Off Days: Everyone’s journey is different, so this section may or may not align with your experiences. I’ve noticed some common ‘triggers’ that occurred for me during these off-days, such as fatigue, insomnia, dehydration, neglecting rest, and not adjusting my day to the situation.
To prevent this from occurring again, one should
(1) recognize the signs of what is happening, including increased stiffness, tremor(s) becoming active, change in your voice, and realizing that a dose may have failed, taking the next dose earlier than usual.
(2) Prioritize self-care by being more mindful and relaxing.
(3) Plan to rest more than usual that day.
(4) Re-confirm your time frame for taking your drugs; count it out very carefully; maybe you were off by a few hours.
(5) Stay hydrated during the day.
(6) Re-evaluate your diet that day. Were you eating something that interfered with carbidopa/levodopa?
(7) Moderate exercise may help your mind reset and support to ease the symptoms.
And (8) If it keeps happening regularly (not twice in 12 years), bring it up with your Neurologist.
Medical Disclaimer: This blog post contains advice and information related to health care. It is not intended to replace medical advice. It should be used as a supplement rather than as a replacement for regular care from your Neurologist.
Final Comments: These events tell me how delicately and precisely balanced my daily carbidopa/levodopa (and NeuPro patch) treatments are. It is essential that I take this therapy at about the same time each day because my body is primed and ready for it. Anything that disrupts this ‘balance’ of carbidopa/levodopa and NeuPro patch, which control these pesky motor symptoms, is crucial to avoid.
Cover Photo Image by Jan Gunnar Nygårdom Pixabay



Hi Frank, Good post and something I have faced many more times than twice. I have experienced ‘off’ days about every 60 days or so, often linked to stress it seems to me. Like you I usually experience the ‘no effect’ with the morning dose having limited or no effect and then I feel fatigued , bradkinsea kicks in and my movement is slow and unstable and i have trouble getting up from a chair. No fun at all!
I have been taking Ryary 4 times per day for 5 years and when I get in an off day (or sometimes just an off period between doses) I take 1/2 of a sinemet and that tends to resolve the problem or at least provide some relief. Since you are taking sinemet I don’t know if that will have the same reaction for you.
Thank for keeping up your blog , I have a list of things to turn. Into blog posts but my apathy always interferes with my plan 😀
Happy New Year
Tom
LikeLike
Tom, thanks for the note. I appreciate your response, and I am certainly sorry this happens to you as frequently as every 60 days or so. It is a terrible feeling, and it just sinks in how dependent our bodies are for the dopamine precursors we take each and every day. Your treatment plan sounds reasonable, it seem that you and I have this problem with the first dose not always working, and then al hell breaks lose. Thanks for the update, take care, Frank
LikeLike
Hi Frank. This sounds possibly related to the Imbalance Theory of PD, which proposes that as your Dopamine decreases in the body, Acetylcholine increases— and that BOTH are involved in PD and its symptoms and especially motor symptoms. Restoring Dopamine a la the added meds you took, can remedy this Imbalance. Acetylcholine activates nerves and too much creates problems, especially with Tremors and muscles. Choline is the base from which Acetylcholine propagates. You can control Choline somewhat with diet by avoiding foods high in it, and thereby reduce Acetylcholine and its negative effects. Arachidonic Acid also reduces Choline as do many PD meds. Have you ever been tested for Choline metabolism or cholinesterases as these modulate Acetycholine? Were the foods you ate on your mega-Off days, high in Choline??? The foregoing is not medical advice for anyone and I am not a doctor. Eugene in Seattle
>
LikeLike
Eugene, thanks a lot for your note I had not considered the imbalance theory of PD and what potental role the other neurotransmitters may contribute to this reaction. I remember writing a blog post about “neurotransmitters” a few years ago, https://journeywithparkinsons.com/2022/12/22/the-complex-role-of-neurotransmitters-in-parkinsons/ and it came across as something much in need of my learning more to better appreciate and understand the interplay of these substances. No, I have not been tested for either choline metabolism or cholinesterease activity, but its easy enough to go to LabCorp and have them do it. Thanks, you given me some homework to furrher my understanding of this complex neurological disease. Thanks again, and take care, Frank
LikeLike